We all agree that a deterioration in the reproductive performance of dairy cows can have a significant impact on the profitability of dairy farms. The immune system has been shown to play an important role in reproduction.
This involvement can be indirect, via the effects of mastitis, metritis, retained placenta and metabolic diseases. However, it can be direct, via the action of immune cells on the ovary. A healthy immune system helps improve the reproductive performance of dairy cattle by reducing the frequency of diseases that affect fertility and maximize the activity of immune cells.
Normally, the cow’s estrous cycle lasts 21 days and is divided into two phases (Figure 1).
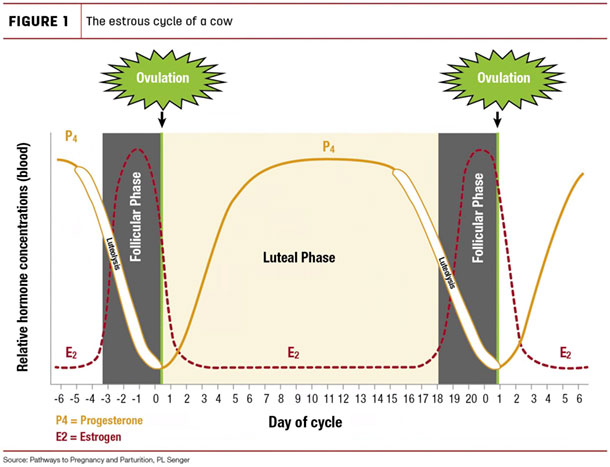
The follicular phase represents 20% of the cycle. During this phase, the preovulatory follicle of the ovary, which contains the oocyte (or ovum), produces estrogen. When estrogen levels are high enough, a surge of luteinizing hormone (LH) is released, triggering ovulation. The luteal phase begins after ovulation, when the follicle turns into a corpus luteum (CL) and produces progesterone to maintain gestation. This phase represents the remaining 80% of the estrous cycle.
Reproductive performance is affected by both the success of conception and pregnancy loss. Typically, gestation lasts 280 days. Up to 40% of pregnancies are lost during the first 17 days of gestation. Early embryonic loss occurs from zero to 15 days of gestation and is usually not detected since the loss of pregnancy at this stage does not delay estrus. Late embryonic loss occurs between 16 and 41 days of gestation and will delay ovulation and thus prolong the estrous cycle. Embryo loss usually occurs before confirmation of pregnancy. Abortion occurs between 42 and 260 days of gestation, and death at birth occurs between 260 days of gestation and birth. The “normal” abortion rates are 3% to 5% per year.
Indirect effects of diseases on dairy cattle reproduction
Infection of the mammary gland affects the structure and functions of the ovaries in addition to being associated with a change in the secretion of reproductive hormones. These effects may be linked to a systemic response of cytokines (released molecules affecting immune cells) which can also lead to the end of gestation. Mastitis is therefore associated with:
- An increase in open days
- Reduced conception rate
- Reduced pregnancy rate
- Higher incidence of early embryonic death
- Greater risk of abortion
Retained placenta is associated with reduced neutrophil function and lower blood levels of interleukin-8 (IL-8, a cytokine that attracts immune cells to sites of infection). These interleukins-8 can then alter the activities of the CL. Retained placenta can therefore also have indirect effects on fertility, in particular causing:
- A decrease in conception rate
- A decrease in pregnancy rate
- An increase in open days
Uterine diseases appear to be issues with the greatest impact on fertility by reducing the rate of ovulation and the size of the CL during the first estrous cycle after calving. Cows with uterine disease also have smaller follicles and lower blood estrogen levels. Uterine diseases also lead to reduced neutrophil function at the time of calving. Uterine diseases, which include metritis and endometritis, are therefore associated with:
- A decrease in conception rate
- Reduced pregnancy rate
- An increase in open days
Metabolic diseases are also associated with impaired reproductive performance. For example, ketosis and clinical and subclinical hypocalcemia lead to an increase in the number of days until the first service as well as a reduction in the rate of conception. As you may know, mastitis, in combination with another metabolic disease, has a greater negative impact on reproduction than any other disease alone.
Direct effects of immune cells on reproduction
Immune cells, mainly neutrophils, macrophages and T cells, are necessary for the reproductive organ to obtain normal ovulation and for the proper functioning of the CL. The activities of these immune cells are regulated by the luteal environment. The neutrophils migrate into the CL (days 1 to 4 of the estrous cycle) in response to the IL-8 produced by the CL. The neutrophil and IL-8 concentrations are low in the middle and toward the end of the luteal phases, but IL-8 is high at luteal regression.
Generally speaking, cortisol (a powerful immunosuppressive hormone released in response to stress) works to block the release and spike of LH from the pituitary gland, which can prevent ovulation. The immune system thus has direct and indirect effects on reproductive performance.
The role of immunomodulators in reproductive health
An immunomodulator is an active agent that helps maintain normal immune activity, despite the various stresses encountered by animals on a daily basis. An effective immunomodulator allows normal and healthy inflammation in response to tissue damage or infection. However, the immunomodulator prevents the inflammatory response from becoming excessive, which can damage tissues in addition to being rather energy-consuming for the proper functioning of the reproductive system, for example.
References omitted but are available upon request by sending an email to the editor.










